December 2025 Edition — COA BulletinClinical Insights
Focusing on symposium summaries, debates, and expert commentary. Stay on top of the latest clinical discussions and perspectives from leading voices in the field.
Innovation and Future Direction of Orthopaedics in Canada and Beyond

Dr. Parth Lodhia (seated far left) with speakers at the ‘Innovation and Future Direction of Orthopaedics in Canada and Beyond’ symposium held during the 2025 Annual Meeting.
Parth Lodhia, MD, FRCSC
2025 Annual Meeting Program Committee Chair
Vancouver, BC
At this year’s COA’s Annual Meeting in Vancouver, BC, I had the privilege of leading a symposium that brought together surgeons from various subspecialties to highlight innovations in their respective fields, and explore what the future holds for orthopaedics in Canada. This included new horizons and opportunities for growth along with specific challenges that may require a renewed mode of thinking and contemporary strategies.
The Future of ACL Reconstruction
Dr. Peter MacDonald (Professor, University of Manitoba)
Dr. MacDonald began with addressing what the future holds for one of the top ten procedures in orthopaedic surgery today: the ACL reconstruction. The challenges facing us include 10-20% graft re-rupture in young athletes, impractical recovery timelines of up to two years, inconsistent return-to-sport, and risk of early osteoarthritis. Dr. MacDonald highlighted advances in surgical techniques with growing high-level evidence for augmentation with the lateral extraarticular tenodesis (LET), internal bracing for graft protection, and the Bridge-enhanced ACL repair (BEAR). There is a parallel advancement in technology with usage of lower profile implants (anchors versus staples) and smaller instrumentation (e.g. nanoscope) to speed up recovery. Biologic enhancements and synthetic or tissue engineered grafts are also continuing to develop. Dr. MacDonald suggested the future would emphasize preservation of the ACL with improved healing along with integration of AI, imaging, and wearable technology to improve outcomes.
The Rise of the Machines – Robotics in Orthopaedic Surgery
Dr. Jesse Wolfstadt (Assistant Professor, University of Toronto)
Dr. Wolfstadt acknowledged that the robots are already here, and here to stay, highlighting how multiple sites across Canada are using robots in arthroplasty. . However, robots may cause information overload and increase case times, the learning curve also has to be considered, and patient expectations need to be temporized. Cost-effectiveness remains a contested topic, particularly in the literature with studies lacking superiority in outcomes from robotics, and various purchasing models that exist in Canadian healthcare to obtain this technology. The future of robotics may very well depend on big data analysis to identify the ideal patient who will benefit the most from it. Finally, AI rose again as a surreal protagonist in helping further total joint replacements.
Spine Surgery Training in Canada
Dr. John Street (Professor, University of British Columbia, President of the Canadian Spine Society)
Dr. Street questioned whether there will be a future for spine in orthopaedics in Canada. Is orthopaedic residency an opportunity or an obstacle for spine training? He underscored the fact that we will have to make some choices, and they may not be easy. There is a shift in the training background of current spine surgeons from orthopaedics to neurosurgery, and there appears to be a significant experience gap between these two disciplines in terms of spine exposure during training, with neurosurgery allowing up to seven times more cases compared to orthopaedics. There is a low number of residents in orthopaedics exploring fellowships in spine. Dr. Street questioned whether it is practical to expect a subspecialty-trained spine orthopaedic surgeon to be hired in a group expecting equal contribution to general orthopaedic call or accepting case costs with new equipment. The question at the heart of this talk was: Is there the will to have a spine residency program? Dr. Street described various statistics that were disparate regarding orthopaedic and neurosurgery programs self-perception of spine surgery requirements. Canada has led the way with more than a decade’s work among dedicated experts to develop a competency-based spine surgery fellowship curriculum that will be available through the Royal College of Surgeons of Canada by August 2026.
Leveraging Private Surgical Centres in Canadian Healthcare: A cross border perspective
Dr. Mahmoud Almasri (Co-Director: Cincinnati Hip Preservation Center) –
Dr. Almasri provided an eclectic perspective with experience in both Canadian and American healthcare systems. The current orthopaedic wait times may create an opportunity for Ambulatory Surgical Centre (ASC) to provide an answer. The ASC can allow for efficiency and quality at the expense of staffing challenges and managing operational costs. Some of the lessons shared from the American perspective included: a focus on volume and standardization, a patient-centric approach, dedicated teams, metrics and outcomes, and leveraging partnerships. This could be a sensitive topic for the Canadian healthcare paradigm. However, Dr. Almasri outlined some solutions with strict contracts to address equity, transparency in contracting to manage a “two-tier” healthcare perception, robust provincial licencing to maintain standards, and incentives in hiring to reduce workflow drain.
Conclusion
This symposium served as a springboard for transformative ideas aimed at evolving orthopaedic care in Canada. It underscored the need to embrace innovation while confronting the realities of our healthcare system. As we look ahead, sharing these advancements with patients will be essential to foster trust and transparency. Equally important are the difficult decisions we must make as a collective—particularly around spine education and the strategic use of ASCs. These choices will be pivotal in addressing disparities in training exposure and alleviating surgical backlogs, ultimately shaping a more responsive and resilient orthopaedic landscape. I would like to thank my co-moderator, Dr Robert McCormack, for his contributions and insights to this session.
Symposium: Innovation and Future Direction of Orthopaedics in Canada and Beyond
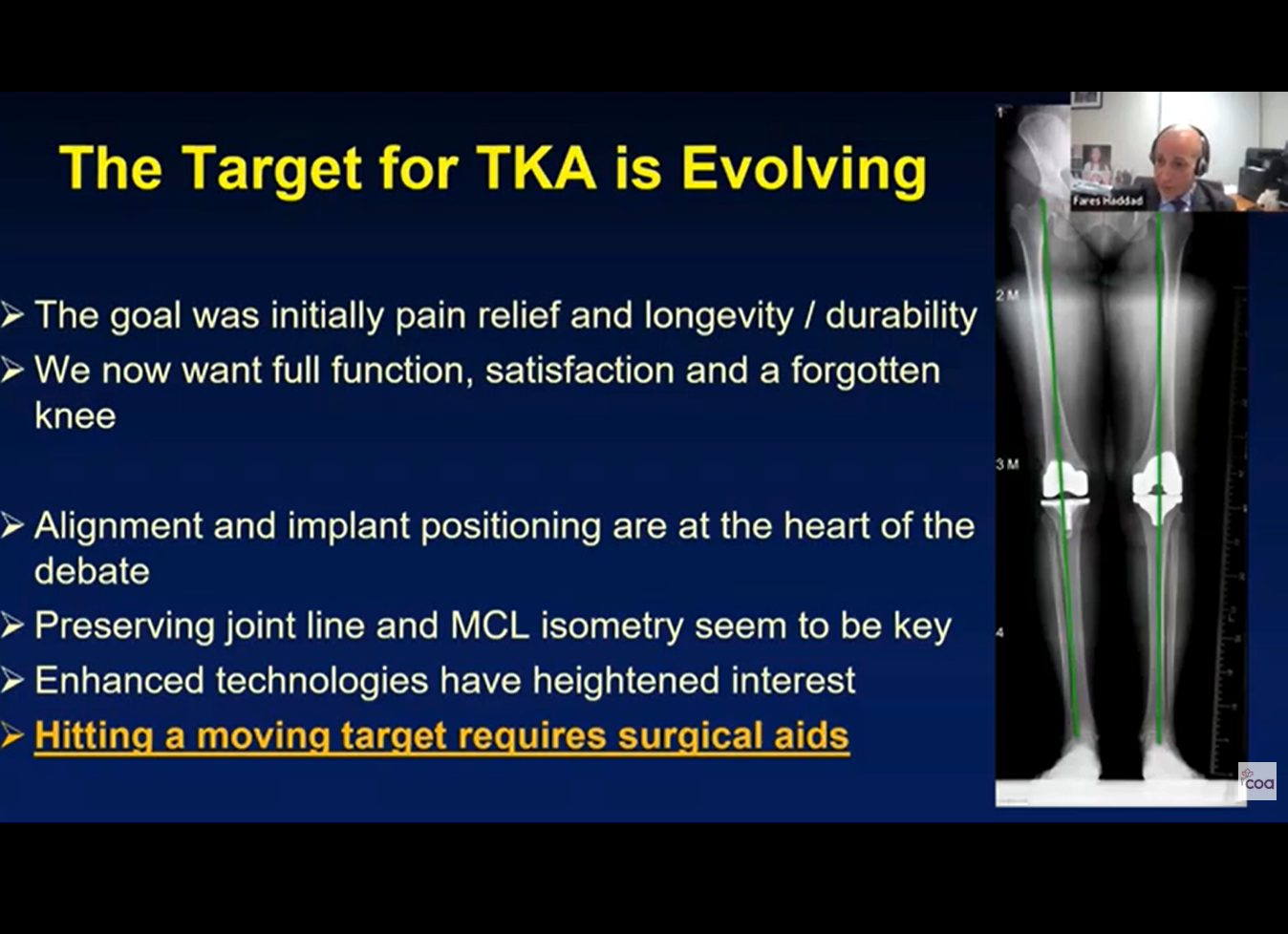
Robotic Hip and Knee Surgery – From Innovation to Evidence Base
 Fares S. Haddad, MBBS MD (Res) MCh (Orth) FRCS (Orth), FFSEM
Fares S. Haddad, MBBS MD (Res) MCh (Orth) FRCS (Orth), FFSEM
University College London Hospitals
London, United Kingdom
Arthroplasty surgery has been life-changing for patients with osteoarthritis over the last few decades. The ability to resolve pain and improve mobility is nothing short of remarkable. Hip arthroplasty was coined ‘the operation of the century’ in the late 1990s, and most lay observers would agree that arthroplasty surgery and cataract surgery stand above most other surgical interventions in their ability to improve quality of life.
Nevertheless, our interventions are still associated with dramatic variation in execution and outcome, and are associated with complications that are expensive for patients and healthcare systems. Errors may occur that are unresolvable and permanently compromise function and mobility. Surgeons, engineers, and scientists working in this area continue to try to improve the planning, execution, implants and bearings, and the outcome of arthroplasty surgery. Most of us have now embraced the digital revolution paralleling other fields where computers now clearly rule. The most straightforward analogy is to the airline industry where we no longer really worry as to who the pilot is, since we know that both the training and the operational side of take-off, flying and landing are largely digitised and rarely falter, and are typically not at the mercy of human error.
Applying the same principles to arthroplasty surgery would require improved planning, with accurate, precise and reproducible intra-operative execution. Robotic surgery has started to deliver some of this, with multiple studies demonstrating improved accuracy and precision of component positioning compared with conventional techniques7. Three-dimensional planning allows us to understand each individual’s anatomy and hence plan on a bespoke basis. At present, three-dimensional planning usually depends on CT-scanning, which brings cost and radiation exposure, but provides a level of detail inaccessible in two-dimensional planning. It also demands an understanding of what is happening in the joint above and below—spine, hip, knee, or ankle. This understanding aids planning for the impact of the limb and body as a whole, rather than viewing an isolated joint. Given large datasets and the power of artificial intelligence, it is only a matter of time before predictive analytics helps determine the optimal path for each patient.
Execution of the case continues to depend on the skill of the surgeon and team, but variation can be reduced with enhanced technologies such as robotics. There are now multiple systems available that vary in planning, execution, and their effectors, but the principle remains that a pre-planned, robotically-executed cut is more accurate and reproducible than one performed manually7.
The initial data on modern robotic systems must not be confused with older systems, often grouped together in meta-analyses. This is further complicated by the emergence of new systems built in the wake of successful CT-based robotic arm platforms. While this reflects strong industry engagement, each system must be evaluated independently. Systematic reviews and meta-analyses of modern robotic platforms, including those for unicompartmental knee arthroplasty (UKA) and total hip arthroplasty (THA), consistently show improved accuracy and reduced outliers compared with manual techniques1,4].
The issue of cost is critical. Healthcare systems must balance the added cost of planning and execution technologies against outcomes delivered. Early data show advantages in the patient journey, including reduced inflammatory response8, greater improvements in knee-specific pain5, improved early functional recovery in some cohorts13, reduced length of stay in certain settings9, and improved precision that may translate into reduced revision risk over time. The most mature data are in unicompartmental knee arthroplasty, where ten-year follow-up demonstrates cost-effectiveness for robotic arm-assisted UKA6. This will likely be followed by similar evidence for total hip and total knee arthroplasty as long-term data accumulate4,10.
Dependence on industry for innovation comes with challenges, including cost pressures, closed platforms and questions about integration, adoption, and evaluation.
We are privileged to deliver highly effective interventions to our patients. Because arthroplasty is already successful, demonstrating incremental improvements can be difficult, posing a challenge for researchers. Nonetheless, continued evolution is essential. Three-dimensional planning and enhanced technologies that optimise intra-operative execution will become increasingly embedded in routine practice in trauma and orthopaedics. Evidence is strongest for hip and knee arthroplasty, but applications are expanding to revision surgery and other joints including shoulder, ankle and spine11,12,14.
Thus far, the introduction of enhanced technologies including robotics has re-awakened interest in defining optimal targets for each patient and personalising interventions, benefitting patient care. It has also generated high-quality research worldwide, such as work on biomechanics3, recovery patterns13, and alignment-specific outcomes14. We must navigate inevitable conflicts and avoid blind adoption of new technologies, ensuring that advances are studied and understood as they evolve. The experience of the past decade suggests robotics are here to stay, and future systems will likely be smaller, easier to use, more integrated, and cost-effective.
References
- Zhang J, Ng N, Scott CEH, et al. Robotic arm-assisted versus manual unicompartmental knee arthroplasty: a systematic review and meta-analysis of the MAKO robotic system. Bone Joint J. 2022;104-B(5):541-548.
- Kayani B, Wazir MUK, Mancino F, et al. The bone trauma and soft-tissue injury classification system in total hip arthroplasty (BOSTI Hip). Bone Joint J. 2024;106-B(9):898-906.
- Tzanetis P, Fluit R, de Souza K, et al. Toward functional reconstruction of the pre-diseased state in total knee arthroplasty. Bone Joint J. 2024;106-B(11):1231-1239.
- Ng N, Gaston P, Simpson PM, et al. Robotic arm-assisted versus manual total hip arthroplasty: a systematic review and meta-analysis. Bone Joint J. 2021;103-B(6):1009-1020.
- Clement ND, Galloway S, Baron J, et al. Patients undergoing robotic arm-assisted total knee arthroplasty have a greater improvement in knee-specific pain. Bone Joint J. 2024;106-B(5):450-459.
- Blyth MJG, Clement ND, Choo XY, et al. Robotic arm-assisted medial compartment knee arthroplasty is cost-effective at ten years. Bone Joint J. 2025;107-B(1):72-80.
- Deckey DG, Rosenow CS, Verhey JT, et al. Robotic-assisted total knee arthroplasty improves accuracy and precision. Bone Joint J. 2021;103-B(6 Suppl A):74-80.
- Kayani B, Tahmassebi J, Ayuob A, et al. Systemic inflammatory response in robotic vs conventional TKA. Bone Joint J. 2021;103-B(1):113-122.
- Fontalis A, Raj RD, Haddad IC, et al. Length of stay after robotic vs conventional arthroplasty. Bone Jt Open. 2023;4(10):791-800.
- Clement ND, Galloway S, Baron YJ, et al. ROAM trial: robotic vs manual TKA. Bone Joint J. 2023;105-B(9):961-970.
- Mancino F, Fontalis A, Grandhi TSP, et al. Robotic conversion of UKA to TKA. Bone Joint J. 2024;106-B(7):680-687.
- Batailler C, Bordes M, Lording T, et al. Improved sizing in robotic-assisted UKA. Bone Joint J. 2021;103-B(4):610-618.
- Hannon CP, Schwabe MT, King J, et al. Recovery after robotic-assisted TKA. Bone Joint J. 2025;107-B(10):1054-1063.
- Manara JR, Whitehouse SL, Marley M, et al. Alignment phenotype and robot-assisted TKA outcomes. Bone Joint J. 2025;107-B(10):1028-1035.
2025 COA National Grand Rounds on Robotic
Hip and Knee Surgery
Ortho Insider Podcast– Season 2, Episode 3
– Prof. Fares Haddad
Oral Antibiotic Therapy for Prosthetic Joint Infections: Evidence, Practice, and Implementation
Gavin Wood MBChB, FRCS (Tr&Orth), FRCSC
Associate Professor, Department of Surgery, McMaster University
Attending Orthopaedic Surgeon, Hamilton Health Sciences
Hamiton, ON
Philip Lam, BScPhm MD MSc FRCPC
Medical Director, Antimicrobial Stewardship
Division of Infectious Diseases, Sunnybrook Health Sciences Centre
Toronto, ON
Prosthetic joint infection (PJI) remains one of the most challenging complications of arthroplasty. In 2025, the Association of Medical Microbiology and Infectious Disease Canada (AMMI Canada), the Canadian Orthopaedic Association (COA), and the Canadian Arthroplasty Society (CAS) released a joint statement1 endorsing the use of highly bioavailable oral antibiotics as a first-line treatment option for bone and joint infections. This article synthesizes evidence from that statement and the accompanying AMMI–COA webinar, highlighting the rationale, clinical framework, and emerging national practice trends surrounding oral antibiotic therapy in orthopaedic infection care.
Introduction
PJIs represent a severe postoperative complication following total hip and knee arthroplasty, leading to substantial patient morbidity, prolonged care, and increased healthcare costs. Population-level data suggest that patients with PJIs experience over a fivefold increase in ten-year mortality risk compared with those with uncomplicated arthroplasty outcomes2. Conventional management involves extended intravenous (IV) antibiotic therapy, often delivered through peripherally inserted central catheters (PICCs), which carry risks of thrombosis, infection, and patient discomfort.
Recent clinical trials and observational studies have demonstrated that oral antibiotic therapy, when appropriately selected, can achieve equivalent outcomes to IV therapy in complex bone and joint infections. The Oral vs IV Antibiotics for Bone and Joint infection (OVIVA) randomized controlled trial established the non-inferiority of oral antibiotic therapy compared with IV regimens, catalyzing a paradigm shift toward less invasive antimicrobial strategies3.
Evidence and Clinical Framework
The AMMI–COA–CAS Joint Position Statement integrates this growing evidence base into practical clinical guidance. It emphasizes that highly bioavailable oral agents—such as fluoroquinolones, linezolid, doxycycline, and rifampin combinations—may be safely and effectively used when specific criteria are met. These include:
- Adequate surgical source control (e.g., debridement, revision, or explant as indicated).
- If a pathogen is isolated, that is susceptible to an appropriate oral agent.
- Absence of other infection foci requiring intravenous therapy.
- Assured gastrointestinal absorption, adherence, and affordability for a 6–12-week treatment course.
Transition to oral therapy may occur as early as 36–72 hours postoperatively, provided the patient is clinically stable and tolerating oral intake. The statement advocates multidisciplinary decision-making involving orthopaedic surgeons, infectious disease physicians, microbiologists, pharmacists, and nursing teams4.
National Practice Patterns
A national survey conducted between October and December 2024 included 51 respondents—21 orthopaedic surgeons and 30 infectious disease or microbiology specialists. While all orthopaedic respondents reported collaboration with infectious disease specialists for PJI management, only a median of 10% of their cases involved predominantly oral antibiotic therapy. In contrast, infectious disease specialists expressed greater comfort with early oral transition, typically after seven days of initial IV therapy. The survey findings underscore the need for continued educational initiatives and interprofessional engagement to standardize practice across disciplines4.
Implementation and Real-World Outcomes
At Sunnybrook Health Sciences Centre, an institutional pathway for early oral transition was implemented in 2022. Between February 2022 and July 2024, 47% of all PJI cases were transitioned to oral therapy by postoperative day seven. Relapse and recurrence rates remained low (7.5%), and most adverse events were mild, primarily gastrointestinal intolerance or rash5. These outcomes align with other real-world implementation studies supporting oral therapy as a safe and cost-effective approach to managing PJIs6.
A representative case from the AMMI–COA webinar5 illustrated this strategy: a 54-year-old man with a Pseudomonas aeruginosa knee PJI successfully transitioned to oral ciprofloxacin by postoperative day five, completing a 12-week course without recurrence at 15 months follow-up. Such experiences reinforce that, with proper selection and monitoring, oral therapy achieves durable infection resolution3.
Discussion
Adoption of oral-first protocols requires institutional support, clinician confidence, and patient engagement. Embedding key checkpoints—microbiologic confirmation, adherence assessment, and follow-up monitoring—into perioperative and discharge processes ensures safe practice4. The approach aligns with principles of antimicrobial stewardship, reduces hospital length of stay, and mitigates PICC-related complications, while maintaining comparable efficacy to IV regimens3,4.
The joint statement1 also promotes continuous data collection and post-discharge surveillance to refine national benchmarks. By integrating oral antibiotic use into existing clinical pathways, Canadian orthopaedic and infectious disease communities are advancing toward a more sustainable, patient-centered model of infection management.
Conclusion
The 2025 AMMI–COA–CAS Joint Statement represents a pivotal step in redefining the standard of care for prosthetic joint infections. Evidence demonstrates that, when supported by surgical control and microbiologic guidance, oral antibiotic therapy is a safe, effective, and resource-conscious alternative to prolonged IV treatment. The transition from bench to bedside will rely on continued collaboration, education, and outcome monitoring, ultimately improving patient recovery and system efficiency in orthopaedic infection care.
References
- Canadian Orthopaedic Association; Association of Medical Microbiology and Infectious Disease Canada. Joint position statement: oral treatment for bone and joint (including prosthetic joint) infections. Ottawa (ON): COA; 2025 Jan 16. Available from: https://coa-aco.org/wp-content/uploads/2025/03/Joint-Statement-Oral-Treatment-for-Bone-and-Joint-Infections.pdf
- Howard JL, Widdifield J, Ravi B, Paterson JM, Marsh JD, Shariff SZ, et al. Association between periprosthetic joint infection and mortality following primary total hip arthroplasty. J Bone Joint Surg Am. 2024 Sep 4;106(17):1400–8. doi:10.2106/JBJS.23.01160.
- Li H-K, Rombach I, Zambellas R, Walker AS, McNally MA, Atkins BL, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019 Jan 31;380(5):425–36. doi:10.1056/NEJMoa1710926
- Lam PW, Lagacé-Wiens P, Gold WL, Peermohamed S, Matukas LM, Poutanen SM, Granger MF, Yamamura D, Leis JA. Use of Oral Antibiotic Therapy for Prosthetic Joint Infections: Considerations for Implementation of Interdisciplinary Practice Changes. J Assoc Med Microbiol Infect Dis Can. 2025 Jun 27;10(2):105-111. doi: 10.3138/jammi-2025-0326. PMID: 40988698; PMCID: PMC12425175.
- Oral antibiotic treatment for prosthetic joint infections [webinar]. Presented by the Canadian Orthopaedic Association; 2024 Nov 28 [cited 2025 Nov 13]. Available from: https://youtu.be/n0gv2hqRr8I?si=dE9YoHL9WnA_S23T
- Azamgarhi T, Shah A, Warren S. Clinical Experience of Implementing Oral Versus Intravenous Antibiotics (OVIVA) in a Specialist Orthopedic Hospital. Clin Infect Dis. 2021 Nov 2;73(9):e2582-e2588. doi: 10.1093/cid/ciaa985. PMID: 32926108.