
December 2025 Edition — COA BulletinAdvocacy in Action
Spotlighting strategic advocacy efforts, and sustainability, diversity initiatives. Explore how the COA is driving change and amplifying the voice of orthopaedics.
Building Safer Recoveries: New IPV Insights and the Future of Support in the Fracture Clinic
 Natalie Fleming, MSW RSW
Natalie Fleming, MSW RSW
Director, IPV Educate Program
McMaster University
Hamilton, ON
For more than a decade, awareness of intimate partner violence (IPV) as a relevant issue within orthopaedic trauma practice has continued to grow. In 2025, IPV is recognized as an essential topic of discussion at international orthopaedic conferences and in educational forums. Within the medical community, the orthopaedic specialty has become a leader in this area and should be proud of that accomplishment. To carry on this legacy, our signature educational program – IPV EDUCATE – has recently been revised and expanded. We have been working to ensure that the material presented uses the latest evidence, best practices, and most effective tools to address IPV. To that end, we would like to provide an update on the latest news from our IPV EDUCATE program.
Our most notable accomplishment in recent years has been the completion of an updated prevalence study on IPV in the fracture clinic which took place at two hospital systems in Hamilton, Ontario. The study included 350 fracture clinic patients and found a high lifetime prevalence of IPV among patients across genders, with especially elevated rates among gender-diverse participants. Some patients, particularly males, disclosed IPV only after their first visit, and about 5% experienced ongoing IPV during the study despite no disclosures to clinical staff. Lifetime history of IPV was associated with poorer return-to-function outcomes, both overall and at work. The results of this study will be published in the Journal of Bone and Joint Surgery shortly, and were presented at this year’s Orthopaedic Trauma Association Annual Meeting1.
We will integrate several important findings from this study into the IPV EDUCATE program going forward. First, gender diversity should be considered when addressing IPV in the fracture clinic, especially when using tools or scripts that focus on women. This study found that non-binary and otherwise gender diverse participants had higher rates of lifetime IPV than cisgender women. Secondly, while this study did not find any injuries that were attributed to IPV and no verbal disclosures of IPV were made to research personnel or clinical staff, approximately 5% of participants were experiencing ongoing violence during their clinical follow-up period. Finally, participants who reported an experience of IPV during their lifetime were found to have a 36% lower rate of return to pre-injury function overall, and a 45% lower rate of return to function with respect to work. These new insights on recovery are particularly important for orthopaedic surgeons to consider as they examine factors contributing to patients’ post-injury function.
Our team continues to present the EDUCATE program to first year surgical residents at McMaster University, which has sparked interest from other surgical disciplines in learning how to integrate IPV assistance into their fields. In response, we now also present IPV EDUCATE to any groups that request this program.
In addition to strengthening the IPV EDUCATE program, we are broadening our focus to address other important factors influencing the health and recovery of fracture clinic patients. To first establish a strong evidence base, we completed preliminary surveys to determine the desires and concerns of both orthopaedic surgeons and patients. This work resulted in two published articles2,3, one of which was presented at the Canadian Orthopaedic Association Annual Meeting in Vancouver this year4. Based on the needs identified in these projects, we have now begun work on a large-scale, batched stepped wedge trial which will incorporate social work services into the outpatient fracture clinic.
This new social worker initiative reflects two important realities: one, fracture clinic patients often present with a wide range of broader health, economic, and social needs, and two, orthopaedic surgeons face significant and increasing demands on their time and cannot reasonably be expected to manage non-orthopaedic health concerns during routine visits. With high patient volume and repeated follow-up visits, fracture clinics provide a unique opportunity to connect patients in need with existing resources and support. With the current trial, we hope to determine if the addition of a social worker to the fracture clinic can enhance patient care while allowing orthopaedic surgeons to remain focused on their core clinical responsibilities.
References
- Fleming N. Hidden Violence: Gender Disparities, Delayed Disclosures, and Poor Clinical Outcomes in Orthopaedic Trauma Patients. Presented at: OTA Annual Meeting; October 18, 2025; Phoenix, Arizona.
- Sprague S, Sheikh A, Fleming N, et al. Prevalence and acceptability of dedicated social work support in the fracture clinic: A survey of orthopaedic trauma surgeons. Scand J Caring Sci. 2025;39(3):e70070.
- Sprague S, Fleming N, Gonsalves M, et al. Patient perspectives on the desirability of social worker support in outpatient orthopaedic trauma clinics. OTA Int. 2025;8(1):e375. doi:10.1097/OI9.0000000000000375
- Fleming N. Prevalence and acceptability of dedicated social work support in the fracture clinic: A survey of orthopaedic trauma surgeons. Presented at: Canadian Orthopaedic Association Annual Meeting; June 11, 2025; Vancouver, BC.
Advancing Equity in Orthopaedics: The COA’s Position on Pregnancy and Parental Leave

Dr. Pascal Thibaudeau was recognized with the 2025 Service to the COA Award for her role on the Board of Directors, and for her leadership of the pregnancy and parental leave statement and study.
Editor’s Note:
In 2019, a proposed Bulletin article planted the seed for a broader conversation about pregnancy and parental leave in orthopaedic surgery. That early initiative—born from personal experience and a desire for clarity—has since evolved into a landmark position statement aimed at supporting surgeons through one of life’s most pivotal transitions.
We spoke with Dr. Pascale Thibaudeau (Lakeshore General Hospital, McGill University), who led the development of this statement, about the journey from informal dialogue to formal policy, the challenges of navigating cultural and institutional variability across Canada, and how this work is helping to reshape the culture of orthopaedics to be more inclusive and equitable – Ed
Q: The topic of pregnancy and parental responsibility in orthopaedics was first raised within the COA community in 2019 as a Bulletin article suggestion that started with a survey to membership. What motivated you to take that early conversation further and lead the development of the COA’s formal position statement, and how did your own experiences help shape its direction?
A: The idea for the initial survey stemmed from my own experience navigating my first pregnancy as a surgeon early in my career. Although my all-male group was very supportive, I found myself facing numerous uncertainties with limited resources to guide me. I had so many practical questions—when should I stop taking call? What about exposure to cement and anesthetic gases in the OR? How long should I take for parental leave without compromising surgical skills or patient care? Should I find a locum to cover my practice?
It quickly became clear that there was a real gap in available information and shared experiences within our community. This inspired me to survey Canadian orthopaedic surgeons to understand how others were managing pregnancy and parental leave. As we navigated the survey results it became very apparent that there was a huge discrepancy in peoples experiences of pregnancy and parenting leave across the country. Furthermore, there were no formal guidelines or rules anywhere in Canada that were relevant to orthopaedic surgeons. Following this, my friend and mentor, Dr. Laurie Hiemstra, invited me to chair a COA working group tasked with developing a formal position statement on pregnancy and parental leave—and I immediately agreed.
Since my first pregnancy, I’ve been contacted by many junior colleagues who were facing similar challenges and looking for guidance. The idea of compiling all this information into a single, evidence-informed document tailored to the Canadian orthopaedic context was deeply motivating. I also felt strongly that achieving gender equity in our profession means normalizing parental leave for everyone—including men. This is well-supported by research showing the benefits of shared parental involvement for both child development and family well-being.
Q: What were some of the surprises or challenges you encountered when drafting the statement, and how were they addressed?
A: One of the main surprises was how limited the available literature was on many of the topics we wanted to address. This meant we needed to rely heavily on the collective expertise and lived experiences of our working group. We intentionally assembled a diverse team—representing different provinces, institutions, career stages, and family environments—to ensure that our recommendations reflected a wide range of perspectives and practice environments.
Another challenge was the variability in cultural norms across Canada. Attitudes and institutional policies regarding pregnancy and parental leave can differ significantly from one province or hospital to another. To address this, we aimed to create a statement that was inclusive, adaptable, and reflective of these regional differences, while still promoting consistency and fairness across the country.
Q: How do you envision this statement influencing policy, residency programs, or workplace culture across Canada?
A: At the institutional level, I hope the statement will encourage departments and hospitals to develop policies that explicitly support pregnancy and parental leave for all surgeons, with clear guidance on safe and reasonable accommodations for pregnant and lactating surgeons.
For residency programs, although most already have policies through their provincial associations, our review revealed wide variability across provinces. We hope this statement will promote more equitable benefits nationwide and ensure that information is easily accessible to all trainees—something that is not currently consistent.
Culturally, while progress is being made, parental leave is still somewhat of a taboo subject in orthopaedics. In what remains a male-dominated field, we aim to normalize the idea that taking parental leave is both acceptable and valuable—for every parent, regardless of gender. Over time, I believe this will help foster a more inclusive, supportive, and balanced professional culture within our specialty.
Shoulder and Elbow Health in Canada: Why We’re Lagging Behind—and How to Fix It

Dominique Rouleau, MD, FRCSC
President, Canadian Shoulder & Elbow Society (CSES)
Professor, Department of Surgery, Université de Montréal
Montreal, QC
Musculoskeletal health in Canada is largely overlooked in a healthcare system that claims to be accessible, but remains highly restrictive. Cost rationalization is necessary, but it is unrealistic and unreasonable in its current form. Some patients are treated at great expense and receive tests or treatments that are not supported by science, while other sick and destitute patients are unable to access treatment for conditions with available, scientifically validated and effective treatment1-6. These spending restrictions have resulted in less access, creating problems that can be seen throughout the country. This rationalization is not based on scientific evidence, but seems to be an easier approach than making targeted political choices. Shortages are reported everywhere and involve orthopaedic surgeons, technical facilities, staff, and administrative personnel to relieve caregivers of non-clinical tasks, the list goes on. We know that patients in need of surgical treatment are disadvantaged compared to patients who need medication to treat their illness. The latter do not have to wait a year to receive a diabetes pill.
Yet, our patients that cannot walk, sleep or work anymore have to wait and do not have access to care. They have to wait twice rather than once; first for an appointment with an orthopaedist to treat their pathology and a second time for an available spot on the surgical wait list. For many pathologies requiring surgery, this comes with a deterioration of the patient’s condition, meaning much greater costs at the time of surgery.
Among patients who are disadvantaged while waiting for orthopaedic care, patients with shoulder or elbow conditions are often more greatly impacted. The data is clear. There is a long-standing policy, supported by the Canadian Institute for Health Information, which prioritizes certain surgeries over others, such as hip and knee replacements, cataract surgery, and heart surgery7,8. Resources are allocated accordingly.
 Let’s take the example of shoulder arthroplasty. Per capita, Canada treats two to three times fewer patients for shoulder replacement surgery than the United States, France, or Australia9,10. This is illustrated by an AI-generated graph using data taken from the literature. Although there is an overall increase in shoulder arthroplasty procedures, the growth appears less pronounced here7,11. There is also a referral bias from primary care professionals, rheumatologists, and physiatrists, as well as a perception bias from patients who believe outcomes are poorer with shoulder arthroplasty than with hip and knee replacements.
Let’s take the example of shoulder arthroplasty. Per capita, Canada treats two to three times fewer patients for shoulder replacement surgery than the United States, France, or Australia9,10. This is illustrated by an AI-generated graph using data taken from the literature. Although there is an overall increase in shoulder arthroplasty procedures, the growth appears less pronounced here7,11. There is also a referral bias from primary care professionals, rheumatologists, and physiatrists, as well as a perception bias from patients who believe outcomes are poorer with shoulder arthroplasty than with hip and knee replacements.
Nothing could be further from the truth! Several studies have shown an improvement in quality of life (SF 36) following shoulder replacement, equivalent to that seen in patients with hip replacement or coronary bypass surgery2,12,13. Furthermore, improvements in tribology and materials for shoulder arthroplasty are on the same scale as for hip/knee arthroplasty, as evidenced by the improvement in implant survival rate following the arrival of the new cross-linked polyethylene and published in the Australian registry10. Following shoulder replacement, the return to golf (80%) is even higher than for patients who have had a knee replacement (70%)14. In addition, shoulder arthroplasty patients have shorter hospital stays, fewer embolic events, lower mortality and morbidity, and require fewer transfusions5,15.
It is also very important to discuss sleeping issues. Between 91% and 97% of patients with end-stage shoulder osteoarthritis experience severe insomnia before surgery. This figure drops to between 13% and 20% postoperatively16,17. It goes without saying that these procedures must be offered to the right patients, after clearly explaining the possible risks and potential benefits. Still, the science is clear: patients with end-stage joint degeneration of the shoulder and elbow deserve care just as much as those with lower limb conditions. They cannot sleep, they are in just as much pain, and their quality of life is just as diminished as that of patients with hip and knee degenerative diseases. Moreover, the success rate and safety of shoulder arthroplasties are on par with those of the hip and knee8,18,19,20.
We can take action:
- Improve orthopaedic education for our fellow physicians and future physicians to counter referral bias.
- Promote the CSES Shoulder & Elbow Course to all Canadian orthopaedic residents to demystify shoulder and elbow pathologies and convey our passion for this growing field.
- Lobby national, provincial, and even hospital decision-makers.
- Use social media to share science-based information on the favourable outcomes of existing treatments for shoulder and elbow pathologies to reduce public perception bias.
- Create and adhere to a national registry for shoulder and elbow arthroplasty.
Based on policies that are not supported by the evidence, with reference biases rooted in the medical community and patients’ perception, Canada is behind compared to other developed countries in the treatment of shoulder and elbow pathologies, as supported by the data on shoulder arthroplasty. We can all act to fight this discrepancy through teaching addressed to all health professionals, political mobilization, scientific vulgarization to the population and reliable Canadian data collection.
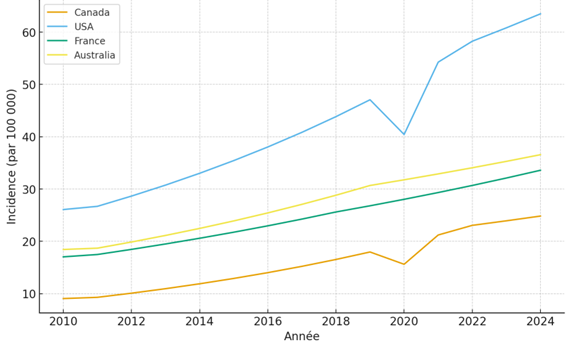
Incidence of shoulder replacement for 100 000 per capita/year. AI-generated content using references provided by the author.
References
1-Bachman D, Nyland J, Krupp R. Reverse-total shoulder arthroplasty cost-effectiveness: A quality-adjusted life years comparison with total hip arthroplasty. World J Orthop. 2016;7(2):123-7. doi: 10.5312/wjo.v7.i2.123.
2-Boorman RS, Kopjar B, Fehringer E, Churchill RS, Smith K, Matsen FA 3rd. The effect of total shoulder arthroplasty on self-assessed health status is comparable to that of total hip arthroplasty and coronary artery bypass grafting. J Shoulder Elbow Surg. 2003;12(2):158-63. doi: 10.1067/mse.2003.18.
3-Carney J, Gerlach E, Plantz MA, Cantrell C, Swiatek PR, Marx JS, Marra G. Short-Term Outcomes After Total Shoulder Arthroplasty in Octogenarians: A Matched Analysis. Cureus. 2021;13(7):e16441. doi: 10.7759/cureus.16441.
4-Curlewis K, Leung B, Sinclair L, Thornhill C, Chan G, Ricketts D. Systemic medical complications following joint replacement: a review of the evidence. Ann R Coll Surg Engl. 2023;105(3):191-195. doi: 10.1308/rcsann.2022.0012.
5-Farmer KW, Hammond JW, Queale WS, Keyurapan E, McFarland EG. Shoulder arthroplasty versus hip and knee arthroplasties: a comparison of outcomes. Clin Orthop Relat Res. 2007;455:183-9. doi: 10.1097/01.blo.0000238839.26423.8d.
6-Hao KA, Cueto RJ, Tams C, King JJ, Wright TW, Parsons M, Schoch BS, Simovitch RW. Quantifying success after anatomic total shoulder arthroplasty: the substantial clinically important percentage of maximal possible improvement. J Shoulder Elbow Surg. 2023;32(11):2303-2309. doi: 10.1016/j.jse.2023.04.010.
7-Wagner ER, Farley KX, Higgins I, Wilson JM, Daly CA, Gottschalk MB. The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg. 2020;29(12):2601-2609. doi: 10.1016/j.jse.2020.03.049.
8-Woolley KA, Chi H, Allahabadi S, Fluet A, Roach C, Ward DT, Wong SE. Sex-Based Differences in the Utilization of Shoulder, Hip, and Knee Arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2023;7(8):e23.00022. doi: 10.5435/JAAOSGlobal-D-23-00022.
9-Lübbeke A, Rees JL, Barea C, Combescure C, Carr AJ, Silman AJ. International variation in shoulder arthroplasty. Acta Orthop. 2017;88(6):592-599. doi: 10.1080/17453674.2017.1368884.
10-Page RS, Alder-Price AC, Rainbird S, Graves SE, de Steiger RN, Peng Y, Holder C, Lorimer MF, Gill SD. Reduced Revision Rates in Total Shoulder Arthroplasty With Crosslinked Polyethylene: Results From the Australian Orthopaedic Association National Joint Replacement Registry. Clin Orthop Relat Res. 2022;480(10):1940-1949. doi: 10.1097/CORR.0000000000002293.
11-Dykhouse, Gabrielle et al. Trends in total shoulder arthroplasty utilization and implant pricing. Seminars in Arthroplasty: JSES. 2025; 35(1): 42-47. doi: 10.1053/j.sart.2024.08.003
12-Horn ME, George SZ, Giczewska A, Alhanti B, Tanner IL, Bolognesi MP. Comparison of adverse events, prescription medication, and costs after hip, knee, and shoulder total joint arthroplasty: a retrospective cohort study. Arthroplasty. 2025;7(1):24. doi: 10.1186/s42836-025-00309-y.
13-Krukhaug Y, Hallan G, Dybvik E, Lie SA, Furnes ON. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. J Shoulder Elbow Surg. 2018;27(2):260-269. doi: 10.1016/j.jse.2017.10.018.
14-Robinson PG, Williamson TR, Creighton AP, Cheng J, Murray AD, Prather H, Dines JS, Gulotta LV, Su EP, Press JM, Hawkes R, Clement ND. Rate and Timing of Return to Golf After Hip, Knee, or Shoulder Arthroplasty: A Systematic Review and Meta-analysis. Am J Sports Med. 2023;51(6):1644-1651. doi: 10.1177/03635465211064292.
15-Lyman S, Sherman S, Carter TI, Bach PB, Mandl LA, Marx RG. Prevalence and risk factors for symptomatic thromboembolic events after shoulder arthroplasty. Clin Orthop Relat Res. 2006;448:152-6. doi: 10.1097/01.blo.0000194679.87258.6e.
16-Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Sleep Disturbance and Anatomic Shoulder Arthroplasty. Orthopedics. 2017;40(3):e450-e454. doi: 10.3928/01477447-20170120-02.
17-Vegas A, Garcia JR, Glener J, Levy JC. Improvement in Sleep Disturbance Following Anatomic and Reverse Shoulder Arthroplasty. J Bone Joint Surg Am. 2023;105(18):1450-1457. doi: 10.2106/JBJS.23.00169.
18-Peri MI, Hopper H, Nelson C, O’Neill CN, Satalich JR, Ernst B, Satpathy J. Total elbow and hip arthroplasties confer greater short-term risk of postoperative complications: a matched cohort analysis of the five major joint arthroplasties. Orthop Rev (Pavia). 2025;17:129554. doi: 10.52965/001c.129554.
19-Roerink AMC, Nelissen RGHH, Holder C, Graves SE, Dunbar M, Bohm E, Grimberg AW, Steinbrück A, Dale H, Fenstad AM, Blom AW, Lenguerrand E, Frampton C, Willems T, Victor J, Espallargues M, Arias-de la Torre J, Ciminello E, Torre M, Pijls BG. Sex-based differences in risk of revision for infection after hip, knee, shoulder, and ankle arthroplasty in osteoarthritis patients: a multinational registry study of 4,800,000 implants. Acta Orthop. 2024;95:730-736. doi: 10.2340/17453674.2024.42183.
20-Rupani N, Combescure C, Silman A, Lübbeke A, Rees J. International trends in shoulder replacement: a meta-analysis from 11 public joint registers. Acta Orthop. 2024;95:348-357. doi: 10.2340/17453674.2024.40948.
Projet de loi 2 et au delà : Défendre nos droits, protéger notre pratique
 Ce qui suit est une adaptation d’une lettre de la Dre Véronique Godbout, présidente de l’Association d’Orthopédie du Québec (AOQ), portant sur l’adoption du projet de loi 2, adopté sous bâillon par le gouvernement du Québec en octobre 2025. Cette législation constitue une réforme majeure de la rémunération des médecins, remplaçant le modèle traditionnel à l’acte par un système liant la compensation à l’inscription des patients, aux taux horaires et aux cibles de performance, tout en réduisant de façon importante les paiements à l’acte.
Ce qui suit est une adaptation d’une lettre de la Dre Véronique Godbout, présidente de l’Association d’Orthopédie du Québec (AOQ), portant sur l’adoption du projet de loi 2, adopté sous bâillon par le gouvernement du Québec en octobre 2025. Cette législation constitue une réforme majeure de la rémunération des médecins, remplaçant le modèle traditionnel à l’acte par un système liant la compensation à l’inscription des patients, aux taux horaires et aux cibles de performance, tout en réduisant de façon importante les paiements à l’acte.
Bonjour à vous tous, membres, collègues et ami(e)s,
Bien que d’habitude j’en profite pour vous souhaiter de belles vacances ou du temps agréable en famille, la situation actuelle rend cette affirmation impertinente. Cependant, malgré les temps difficiles, il reste important de s’accrocher aux moments et aux personnes qui ont la capacité de vous rendre heureux et de vous distraire des actualités. Le niveau actuel de stress et d’anxiété est à un niveau inégalé, et la préservation de votre santé doit rester prioritaire.
Comme vous le savez bien, le dernier coup de massue du gouvernement est l’adoption sous bâillon de la Loi 2, ayant pour objectif de modifier la rémunération des médecins. Cependant, comme vous l’avez constaté, cette loi est liberticide et représente une atteinte fondamentale à nos droits et libertés.

La présidente de l’AOQ, Dre Véronique Godbout, ainsi qu’une membre de l’ACO, Dre Stephanie Hinse, ont pris part aux manifestations qui ont rassemblé des dizaines de milliers de médecins à travers la province plus tôt cet automne.
Depuis la nuit fatidique du 24 octobre, beaucoup de nouvelles, de manifestations, de surprises, etc. se sont produites. La FMSQ fait un travail exceptionnel sur tous les plans : être à l’écoute des déclarations politiques, étudier la Loi pour la décrypter et en comprendre toutes les subtilités, contester juridiquement la Loi, consulter ses membres et ses présidents, mais surtout, informer les membres. Si vous ne l’avez pas encore fait, je vous encourage à lire les Infos Négos envoyés régulièrement depuis les dernières semaines. Vous y trouverez toutes les nouvelles les plus récentes et les rebondissements inattendus. Les aspects les plus nébuleux de cette Loi sont les modalités d’application et l’impact financier potentiel. Actuellement, il est impossible de prédire exactement ce qu’il en sera.
En date du 11 décembre 2025, nous apprenons que la Loi 2 sera suspendue jusqu’en février le temps de négocier. Les rencontres entre Dr Oliva et Francois Legault ont donc permis de suspendre la Loi pour que la FMSQ se remette à la Table des négociations. Le mandat est clair – nous n’accepterons pas une entente inacceptable seulement pour éloigner la Loi 2. La possibilité que l’application de la Loi soit effective en février est donc toujours présente si aucune entente de principe ne survient d’ici là.
Au niveau des démarches juridiques intentées par la FMSQ, voici un petit résumé vulgarisé :
- Demande de sursis et d’interprétation des clauses liées aux actions concertées et aux pénalités
Par exemple : Un couple quitte la province pour travailler ailleurs au Canada- Interprétation FMSQ : ils pourraient être passible des pénalités prévues à la Loi.
- Interprétation du Procureur général : aucune pénalité ne s’appliquerait si le départ n’a pas pour objectif de nuire à l’accès aux soins
- Objectif de la FMSQ : faire invalider rapidement les dispositions les plus restrictives de la Loi 2.
- Résultat : Le juge Me Nollet a refusé de trancher, estimant que sa décision pourrait être contestée et donc ne ferait progresser aucune des parties.
-
Demande de sursis interlocutoire visant à reporter l’application de la Loi 2
Il était prévu qu’à partir de la mi-décembre, la demande de la FMSQ soit débattue devant les tribunaux afin de soutenir que certains articles de la Loi 2 ne peuvent entrer en vigueur le 1er janvier, compte tenu de leurs nombreux effets préjudiciables (atteintes aux droits et libertés, absence de négociation de bonne foi des conditions salariales, etc.). Cette requête visait aussi la suspension des mesures financières punitivesAvec la suspension temporaire de la Loi 2, il reste incertain ce qu’il advient de cette demande.Avec la suspension temporaire de la Loi 2, il reste incertain ce qu’il advient de cette demande.
-
Contestation judiciaire sur le fond de la Loi 2
Une contestation judiciaire sur le fond de la Loi 2 a également déjà été déposée, mais il s’agit d’une procédure n’ayant pas le même degré d’urgence et qui ne sera pas entendue avant plusieurs mois.Les deux premières démarches visaient à déterminer si une suspension était nécessaire afin de préserver l’intégrité du réseau de la santé. La suspension temporaire rend ces actions moins pertinentes pour l’instant, mais il faut rappeler qu’elle n’est que provisoire : la Loi pourrait entrer en vigueur dès la fin février 2026.
Les exemples que vous avez transmis à la FMSQ font partie de ces dossiers juridiques et aident à étoffer le dossier. Advenant une application de la Loi 2, l’action #3 est toujours en cours et pourra être entendue en 2026 – du moins, c’est ce que l’on anticipe, même si la Cour ne la considère pas comme urgente.
Concernant les impacts concrets sur notre pratique advenant une application de la Loi 2
Nous devons anticiper une réduction minimale de 13,04 % sur tous les codes. L’abolition du supplément de consultation touchera différemment chacun selon son type de pratique; les médecins travaillant principalement en cabinet pourraient subir des pertes allant jusqu’à 40 %. Plusieurs cliniques médicales et radiologiques ont déjà annoncé des fermetures, jugeant leur modèle financier non viable
L’analyse préliminaire de la FMSQ montre que les pertes résultent de la combinaison de trois mesures :
- La diminution généralisée des tarifs de 13,04 % dès l’application de la Loi 2
- Le retrait des suppléments de consultation
- La révision des tarifs en télémédecine, dont l’impact demeure limité pour nos membres
Au total, ces changements représentent une diminution d’environ 17 % de l’enveloppe annuelle, soit des pertes pouvant approcher 100 000 $ par année pour plusieurs d’entre nous, et jusqu’à 38 % selon le profil de pratique. Il est essentiel de nommer cette réalité sans détour : de telles réductions bouleversent nos vies. Elles remettent en question des projets familiaux, retardent des plans de retraite pourtant bien établis, fragilisent des engagements financiers pris de bonne foi et forcent plusieurs collègues à revoir entièrement leur équilibre personnel et professionnel.
Dans ce contexte, il est tout à fait normal que chacun évalue ses options pour préserver son équilibre et son bien-être. Le PAMQ n’a jamais été autant en demande, ce qui illustre l’ampleur des impacts anticipés.
Cibles et contente orthopédique
Rappelons-nous que l’orthopédie a été la spécialité la plus touchée suite à la pandémie avec une explosion des listes d’attente en chirurgie et des listes impressionnantes de consultations au CRDS. Bien que le nombre de patients en attente de chirurgie depuis plus d’un an a beaucoup diminué dans la dernière année, cette amélioration s’est faite au détriment des autres patients puisqu’il n’y a pas eu d’augmentation significative des ressources disponibles. Il manque toujours de lits, de personnel para médical varié, etc. L’amélioration s’est aussi beaucoup produite grâce à votre travail acharné pour implanter et améliorer les protocoles de chirurgies d’un jour pour les arthroplasties dans vos hôpitaux. Comme nous ne vivons pas dans un monde de licornes, il est évident que le Ministre Dubé ne trouvera pas du jour au lendemain les ressources nécessaires pour atteindre des cibles qui resteront donc inatteignables. Il faut alors assumer que la coupure de 13,04 % ne sera probablement jamais retournée dans nos poches.
Pendant que l’Ontario obtient une hausse de 10 % et le Nouveau-Brunswick plus de 12 %, le Québec fait face à une réduction de plus de 13 %, ce qui nuit fortement à son attractivité. Avec un nombre de finissants historiquement bas et aucune hausse significative prévue avant cinq ans, nous nous dirigeons vers une période difficile. Un sondage récent indiquait que 22 % envisagent une retraite anticipée, plus de 40 % une pratique partielle au privé, et 21 % une réorientation (étant trop jeune pour une retraite). En plus de départs anticipés à la retraite, d’exode ou de modifications de pratiques, nous devrons faire face à une mauvaise planification des effectifs et une relève qui se fera attendre.
Tout cela survient alors que les besoins populationnels en orthopédie continuent d’augmenter.
Suite des démarches
Pour conclure sur le sujet de la Loi 2, la FMSQ a pour mandat de ne retourner à la table de négociation que si :
- L’application de la Loi 2 est suspendue, et;
- Que l’actuel ministre de la Santé est exclu des négociations.
Il semble donc que ces deux conditions soient atteintes et que nous retournerons à la Table de négociations. La FMSQ entend organiser un webinaire vers le 18 décembre pour informer les médecins spécialistes des conséquences de l’entrée en vigueur de la Loi 2. Bien que suspendue, nous croyons que ce webinaire reste nécessaire. De notre côté, nous tiendrons une séance d’information et de questions le 15 décembre 2025.
Mot de conclusion
Dans cette période d’incertitude, je vous invite à faire preuve de bienveillance, à écouter vos pairs, et à ne pas oublier de prendre du temps pour vous. Prenez les mesures nécessaires pour préserver votre santé physique et psychologique. Si vous vous sentez dépassé par les événements, sachez que vous n’êtes pas seul. Le rassemblement au centre Bell l’a démontré : nous sommes tous dans le même bateau (en train de couler j’en conviens). Continuez à faire entendre votre voix, à dénoncer les aberrations du système qui nous empêchent de pratiquer une médecine optimale, au niveau de notre compétence et de notre expertise. Votre voix porte énormément, et les médias ainsi que la population est beaucoup plus ouverte aux témoignages du terrain qu’à ceux des « représentants syndicaux ». N’hésitez donc pas à vous manifester et à répondre favorablement aux demandes d’entrevue que vous recevez. Nous, ainsi que la FMSQ, demeurons disponibles pour vous soutenir.
Véronique Godbout, MD, FRCSC
Présidente, l’Association d’Orthopédie du Québec
Bill 2 and Beyond: Defending Our Rights, Protecting Our Practice
 The following is an adaptation of a letter from Dr. Véronique Godbout, President of the Quebec Orthopaedic Association (QOA), addressing the adoption of Bill 2, passed under closure by the Quebec government in October 2025. This legislation introduces a sweeping reform of physician remuneration, replacing the traditional fee‑for‑service model with a system that ties compensation to patient registration, hourly rates, and performance targets, while significantly reducing fee‑for‑service payments across the board.
The following is an adaptation of a letter from Dr. Véronique Godbout, President of the Quebec Orthopaedic Association (QOA), addressing the adoption of Bill 2, passed under closure by the Quebec government in October 2025. This legislation introduces a sweeping reform of physician remuneration, replacing the traditional fee‑for‑service model with a system that ties compensation to patient registration, hourly rates, and performance targets, while significantly reducing fee‑for‑service payments across the board.
Hello to all members, colleagues, and friends,
Although I usually take this opportunity to wish you a wonderful vacation or enjoyable time with your families, the current situation makes such a message feel out of place. However, despite these difficult times, it remains important to hold on to the moments and the people who can bring you happiness and help distract you from the news. The current level of stress and anxiety is unprecedented, and protecting your health must remain a priority.
As you know, the government’s latest heavy‑handed move was the forced adoption of Bill 2, which aims to modify physicians’ remuneration. However, as you have noticed, this law is deeply restrictive and represents a fundamental violation of our rights and freedoms.

QOA President, Dr. Véronique Godbout and COA Member, Dr. Stéphanie Hinse, participated in demonstrations with tens of thousands of physicians that were held across the province earlier this fall.
Since the fateful night of October 24, many developments, demonstrations, and surprises have occurred. The Federation of Medical Specialists of Quebec (FMSQ) has been doing exceptional work on all fronts: monitoring political statements, studying the law to decipher and understand all its nuances, legally challenging the legislation, consulting its members and presidents, and above all, keeping members informed. If you haven’t done so yet, I encourage you to read the “Infos Négos” updates sent regularly over the past few weeks. You will find the latest news and unexpected developments there. The most unclear aspects of this law are its implementation mechanisms and the potential financial impact. At this time, it is impossible to predict exactly what will happen.
As of December 11, 2025, we have learned that Bill 2 will be suspended until February to allow time for negotiations. Meetings between Dr. Oliva and François Legault have therefore resulted in the suspension of the law so that the FMSQ can return to the bargaining table. The mandate is clear: we will not accept an unacceptable agreement simply to push Bill 2 aside. The possibility that the law could still come into effect in February remains if no agreement is reached.
Regarding the legal actions undertaken by the FMSQ, here is a brief, simplified overview:
- Request for a stay (suspension) and for interpretation of the clauses related to concerted actions and the associated penalties
For example, a couple decides to leave the province to work elsewhere in Canada- FMSQ interpretation: they could be subject to the penalties mentioned if they decided to leave the province.
- Interpretation of the Attorney General: they would not be subject to penalties if their intention was not to harm access to care.
- Purpose of the FMSQ’s action: to urgently invalidate the most restrictive and rights‑limiting aspects of Bill 2.
- Outcome: Justice Nollet refused to rule, as his decision could then be appealed, leaving neither party any further ahead.
-
Interlocutory stay application seeking to postpone the implementation of Law 2
It had been planned that, starting in mid‑December, the FMSQ’s application would be argued before the courts in order to demonstrate that certain articles of Law 2 could not come into force on January 1, given their numerous harmful effects (violations of rights and freedoms, lack of good‑faith negotiation of salary conditions, etc.). This application also sought the suspension of the punitive financial measures.Given the temporary suspension of Bill 2, it is unclear what will happen to this request.
-
Judicial challenge on the merits of Bill 2
A judicial challenge on the merits of Law 2 has also already been filed, but this procedure is less urgent and will not be heard for several months.The first two actions aimed to determine whether a suspension was necessary to preserve the integrity of the health‑care system. The temporary suspension makes these steps less relevant for the moment, but it is important to remember that it is only provisional: the Law could come into force as early as the end of February 2026.
The examples you provided to the FMSQ are part of these legal files and help strengthen the case. Should Law 2 be implemented, action #3 remains active and could be heard in 2026 — at least, that is what is anticipated, even though the Court does not consider it urgent.
Regarding the concrete impacts on our practice should Bill 2 be implemented:
We should anticipate a minimum cut of 13.04% across all billing codes. The elimination of the consultation supplement will affect each of us differently depending on our practice type; physicians working primarily in office-based settings could face losses of up to 40%. Several medical and radiology clinics have already announced closures, judging their financial model no longer viable.
Preliminary analysis by the FMSQ shows that these losses stem from the combination of three measures:
- the across‑the‑board 13.04% reduction in fees upon implementation of Law 2
- the elimination of consultation supplements
- the revision of telemedicine fees, whose impact remains limited for our members
Combined, these changes result in an approximate 17% reduction in the annual envelope, translating into losses approaching $100,000 per year for many of us, and up to 38% depending on the practice profile. It is important to state this reality plainly: such reductions profoundly disrupt our lives. They call into question family plans, delay well‑established retirement timelines, weaken financial commitments made in good faith, and force many colleagues to completely reassess their personal and professional balance.
In this context, it is entirely normal for each of us to consider our options in order to preserve our stability and well‑being. Demand for the PAMQ (programme d’aide aux médecins du Québec) has never been higher, which clearly illustrates the magnitude of the anticipated impacts.
Targets and Orthopaedic Context
Let’s remember that orthopaedics has been the specialty most affected since the pandemic, with an explosion in surgical waitlists and exceptionally long consultation lists at the CRDS (Centre de répartition des demandes de services, or Service Request Management Centre). Although the number of patients waiting more than a year for surgery has decreased significantly over the past year, this improvement came at the expense of other patients, as there has been no meaningful increase in available resources. There is still a shortage of beds, diverse paramedical staff, and other essential resources. Much of the progress achieved is the result of your hard work in implementing and improving same‑day surgery protocols for arthroplasties in your hospitals.
Since we do not live in a world of unicorns, it is clear that Minister Dubé will not suddenly find the resources needed to meet targets that are, in reality, unattainable. We must therefore assume that the 13.04% cut will likely never be restored.
While Ontario has obtained a 10% increase and New Brunswick more than 12%, Quebec is facing a reduction of over 13%, which severely undermines its attractiveness. With a historically low number of graduates and no significant increase expected for another five years, we are heading into a difficult period. A recent survey indicated that 22% are considering early retirement, more than 40% are contemplating partial private practice, and 21% are considering a career shift (being too young to retire). In addition to early retirements, departures, and changes in practice patterns, we will also face poor workforce planning and a delayed succession.
All of this is happening while population‑level needs in orthopedics continue to rise.
Next Steps
To conclude on the topic of Law 2, the FMSQ has been mandated to return to the bargaining table only if:
- the application of Law 2 is suspended, and
- the current Minister of Health is excluded from the negotiations.
It appears that both conditions have now been met, and that we will therefore be returning to the bargaining table. The FMSQ plans to hold a webinar around December 18 to inform medical specialists about the consequences of Law 2 coming into force. Even though the law is currently suspended, we believe this webinar remains necessary. On our end, we will hold an information and Q&A session on December 15, 2025.
Closing Remarks
In this period of uncertainty, I encourage you to show kindness, to listen to your colleagues, and to remember to take time for yourselves. Take the steps needed to protect your physical and psychological health. If you feel overwhelmed by the situation, know that you are not alone. The gathering at the Bell Centre made it clear: we are all in the same boat (albeit one that is sinking, I admit).
Continue to make your voices heard and to speak out against the system’s shortcomings that prevent us from practicing medicine at the level of our competence and expertise. Your voice carries tremendous weight, and both the media and the public are far more receptive to frontline testimony than to that of “union representatives.”
So please do not hesitate to speak up and to accept interview requests when they come your way. We, along with the FMSQ, remain available to support you.
Véronique Godbout, MD, FRCSC
President, Quebec Orthopaedic Association